Scientists and researchers have their odd ways of solving problems, and when they team up with one of the biggest biotech companies, their ideas can go beyond research papers—and become real-world solutions we get to see.
Brief History of Pertuzumab
Pertuzumab (Parjeta) is a clear example of a scientific and marketing genius. It entered the market in 2012 to treat breast cancer in combination with Herceptin (trastuzumab) and one of the taxenes (a group of chemotherapeutic agents).
So what is so interesting about pertuzumab?
Genentech has marketed Herceptin (Trastuzumab) in 1998. It was a scientific and clinical breakthrough. Trastuzumab became the first monoclonal antibody to target the HER-2 receptor on the surface of the cancer cells. It made the company billions of dollars and cemented itself as a standard of care.
Trastuzumab secret
Although Herceptin delivered the expectation of improving clinical outcomes for many patients with breast cancer, scientists were particularly unsettled with one trastuzumab issue – they do not exactly know how it works!
Trastuzumab and HER2
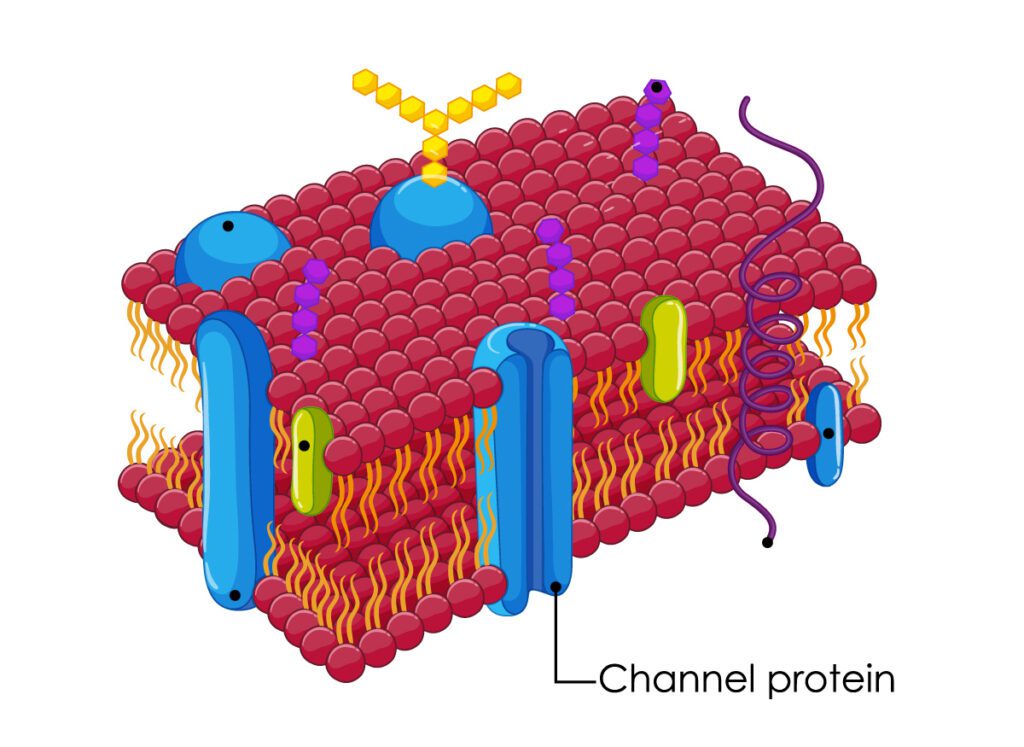
Trastuzumab binds the Human Epidermal Growth factor Receptor-2 ( HER-2), which is found in every fifth case of breast cancer. Breast cancer cells express HER-2 to survive, grow, and spread, which makes HER-2 an attractive target for targeted agents and chemotherapy.
The tigh has formed, but the process, which follows next is still a subject of the scientific debate. The research community has identified four most probable scenarios:
- It stops the process of heterodimerization of HER-2;
- It adds phosphorus to the HER-2 protein;
- It facilitates the removal of the HER-2 from the cell surface;
- It attracts immune cells that destroy cancer.
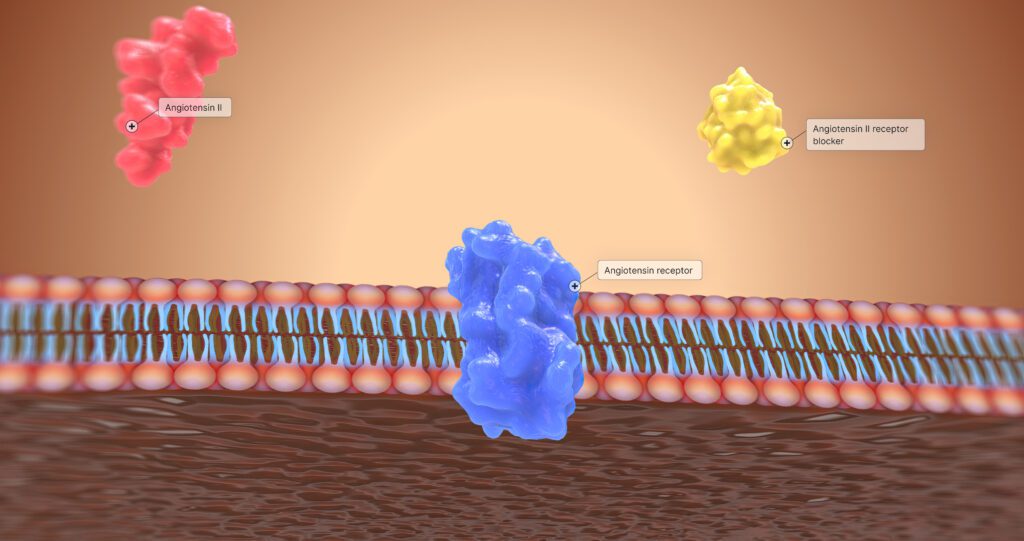
Heterodimerization
HER-2 is a unique protein in the family of four tyrosine kinases. All representatives exist in two forms:
- Monomer or inactive form.
- Dimer form or active form. The dimer is essentially two monomers bonded together.
HER-2 cannot cannot bind another HER-2, it can only bind other members of the family (usually HER-1 or HER-3). The process is called heterodimerization, and it is crucial for activating cancer growth, expansion, and
Another way, scientists thought Herceptin works is by invoking a phosphorylation of the HER-2 receptor. Phosphorylation is adding a phosphorus residue to one of the amino acids (usually tyrosine). Phosphorylation makes HER-2 less stable and overall leads to a better prognosis for cancer patients.
More recent studies suggest that trastuzumab facilitates endocytosis of the HER-2 receptor – the cancer cells just swallow their receptors removing it from the surface.
Finally, some scientists believe trastuzumab binds the HER-2 receptor and “calls” the immune system to fight cancer cells. This theory is supported by microscopic evidence – cancer tissues treated with trastuzumab, were heavily infiltrated by different immune cells.
Pertuzumab is an “open book” for researchers.
Similar to trastuzumab, pertuzumab is a monoclonal antibody, that binds HER-2 receptor. Unlike its “enigmatic friend, trastuzumab’s mechanism of action is clear – upon binding the target, it prevents dimerization of HER-2.
Pertuzumab in action
Pertuzumab Basics
Pertuzumab is a humanized monoclonal antibody primarily used in cancer therapy. It targets the HER2 receptor, playing a crucial role in inhibiting tumor growth in HER2-positive breast cancer. Understanding its classification and properties helps in appreciating its impact on treatment.
Classification and Overview
Pertuzumab is classified as a recombinant humanized monoclonal antibody. It specifically targets the extracellular domain II of the HER2 receptor.
This mechanism blocks dimerization with other HER family receptors, inhibiting downstream signaling pathways. Pertuzumab is used in combination with trastuzumab and chemotherapy to enhance therapeutic efficacy.
It is particularly effective in treating metastatic breast cancer and has been shown to improve survival rates in patients.
Chemical and Biological Properties
Pertuzumab has a molecular weight of approximately 148 kDa. It is composed of 4 heavy chains and 4 light chains, which form its unique structure.
The drug is produced using recombinant DNA technology in Chinese hamster ovary cells. Pertuzumab’s stability and half-life allow for effective dosing in clinical settings.
Administration is typically via intravenous infusion, with dosages tailored to the patient’s specific needs. Understanding these properties is essential for optimizing its therapeutic use.
Mechanism of Action
Pertuzumab acts through a specific mechanism involving multiple interactions with HER2 receptors, playing a significant role in cancer treatment. Its primary functions include binding to HER2 receptors, inhibiting dimerization, and enhancing immune responses.
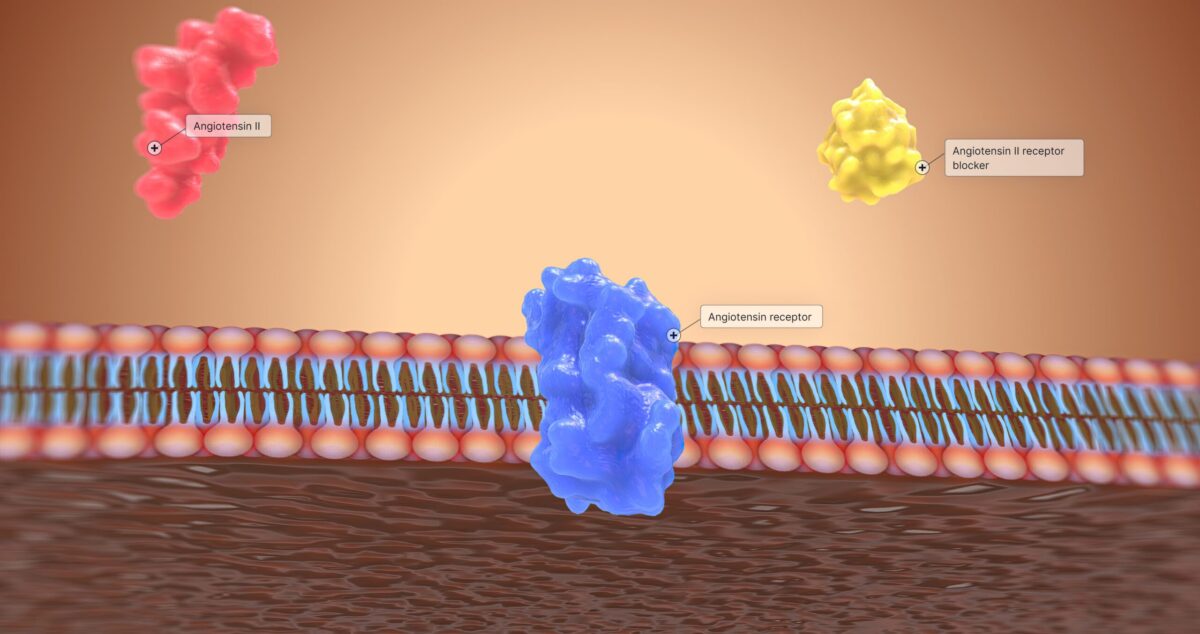
Binding to HER2 Receptors
Pertuzumab binds selectively to the extracellular domain of the HER2 receptor. This process blocks the receptor’s ability to interact with other molecules involved in cell signaling.
The binding alters how cancer cells receive growth signals. By preventing HER2 signaling, pertuzumab reduces proliferation and survival of these cancerous cells. Clinically, this provides an effective strategy in treating HER2-positive breast cancer.
Inhibition of HER2 Dimerization
Dimerization is crucial for HER2 function. Pertuzumab prevents HER2 from forming dimers with other related receptors, such as HER3. This inhibition is essential because dimerization activates pathways that promote tumor growth.
Blocking this process disrupts signaling networks that would otherwise support cancer cell survival. The result is decreased cell division and increased apoptosis in tumor cells, enhancing therapeutic outcomes.
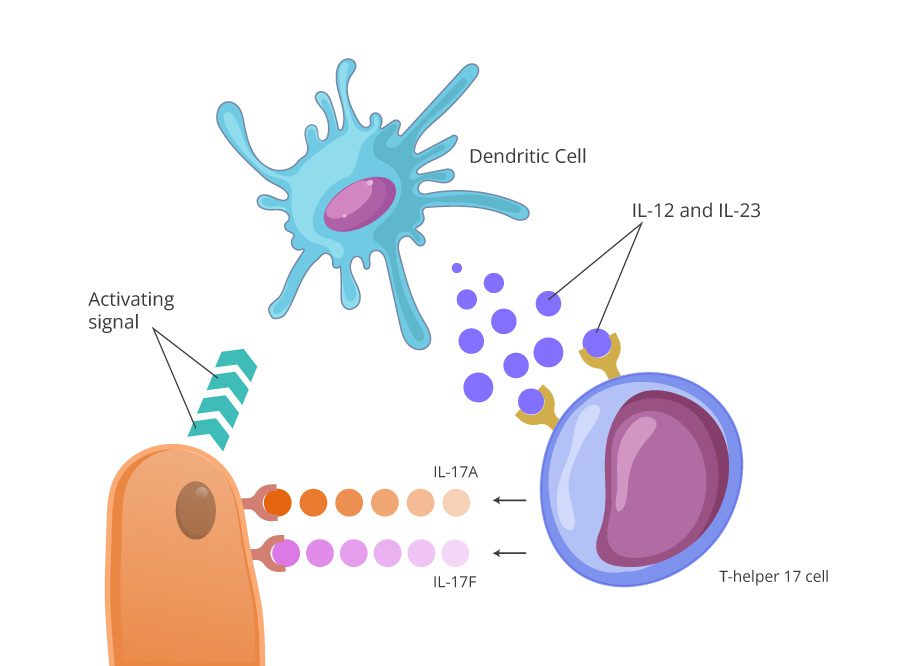
Activation of Antibody-Dependent Cellular Cytotoxicity
Pertuzumab also enhances immune response through antibody-dependent cellular cytotoxicity (ADCC). The binding of pertuzumab to HER2 helps recruit immune cells.
These immune cells, such as natural killer (NK) cells, are activated to target and destroy HER2-expressing cancer cells. This mechanism provides an additional layer of antitumor activity, contributing to the effectiveness of pertuzumab in HER2-positive cancers.
Trastuzumab with Pertuzumab
The combination of trastuzumab and pertuzumab has become an important strategy in the treatment of HER2-positive breast cancer. This section explores how these two therapies work together to improve patient outcomes.
Breast Cancer Treatment
Trastuzumab, a monoclonal antibody, specifically targets the HER2 receptor, blocking signaling pathways that promote cancer cell growth. Pertuzumab also targets HER2 but binds to a different site, preventing receptor dimerization, which is essential for activating downstream signaling.
When used together, these agents enhance therapeutic efficacy. Studies have shown that their combination leads to improved progression-free survival rates in patients with early-stage and metastatic HER2-positive breast cancer.
This dual blockade not only targets the cancer more effectively but may also reduce the chances of resistance. The synergy between trastuzumab and pertuzumab represents a significant advancement in personalized cancer treatment, offering hope to many patients.
Clinical Efficacy
Pertuzumab has demonstrated significant clinical efficacy in the treatment of certain cancers, notably HER2-positive breast cancer. Its unique mechanism of action enhances the effectiveness of standard therapies. This section details relevant clinical trials, survival and response rates, and its comparison with other treatments.
Relevant Clinical Trials
Several key clinical trials have assessed the efficacy of pertuzumab in combination with trastuzumab and chemotherapy. The pivotal study, CLEOPATRA, involved over 800 patients and reported a significant improvement in progression-free survival (PFS). Patients receiving pertuzumab showed a median PFS of 18.5 months, compared to 12.4 months for those receiving the control regimen.
Clinical Data
Moreover, results from the APHINITY trial indicated a similar benefit in the adjuvant setting, where pertuzumab combined with trastuzumab increased the invasive disease-free survival compared to trastuzumab alone. These findings underline the drug’s role in improving outcomes for patients with HER2-positive breast cancer.
Survival and Response Rates
Pertuzumab has significantly enhanced survival rates among treated patients. In the CLEOPATRA trial, the addition of pertuzumab resulted in an overall survival rate of 86% at three years, compared to 84% for the control group. This difference highlights its impact on long-term outcomes.
Response rates also reflect its efficacy. In the APHINITY trial, a notable 94.1% of patients exhibited a pathologic complete response when treated with both pertuzumab and trastuzumab preoperatively. These figures demonstrate its effectiveness in promoting favorable responses.
Comparison to Other Treatments
When compared to traditional therapies, pertuzumab shows improved efficacy in HER2-positive cancer management. For instance, the combination of pertuzumab and trastuzumab performs better than trastuzumab alone, resulting in improved PFS and overall survival rates.
Other HER2-targeted therapies, such as lapatinib, provide different mechanisms but often have lower response rates. Studies have shown that patients on pertuzumab plus chemotherapy benefit from a robust treatment regimen, positioning it as a critical option in therapy for HER2-positive cancers.
Future Directions in Research
Research on pertuzumab continues to expand, focusing on ongoing clinical trials and exploring potential new therapeutic indications. These efforts aim to enhance understanding of its effectiveness and broaden its application.
Ongoing Clinical Trials
Numerous clinical trials are currently assessing the efficacy and safety of pertuzumab in various cancer types. One significant trial is investigating its use combined with trastuzumab and chemotherapy for HER2-positive breast cancer.
Additional studies are exploring the sequencing of pertuzumab with other novel agents, such as immune checkpoint inhibitors, to evaluate potential synergistic effects. This research may offer insights into improved patient outcomes through combination therapies.
Researchers are also examining different dosing regimens and administration methods to optimize treatment schedules. These trials aim to understand patient response based on specific biomarkers and genetic profiles.
Potential New Indications
Beyond breast cancer, there is growing interest in using pertuzumab for other malignancies. Investigations are underway to determine its effectiveness in gastroesophageal cancers, where HER2 overexpression is present.
Researchers are also testing pertuzumab in combination with targeted therapies for lung and ovarian cancers. Exploring its role in these contexts may uncover new therapeutic avenues for patients who have limited options.
Additionally, studies are exploring pertuzumab’s potential in neoadjuvant settings, where it could be used before surgery to shrink tumors. This could enhance surgical outcomes and improve long-term prognosis for patients.