Nivolumab helps your immune system fight cancers by blocking the tumor’s ability to evade the immune response.
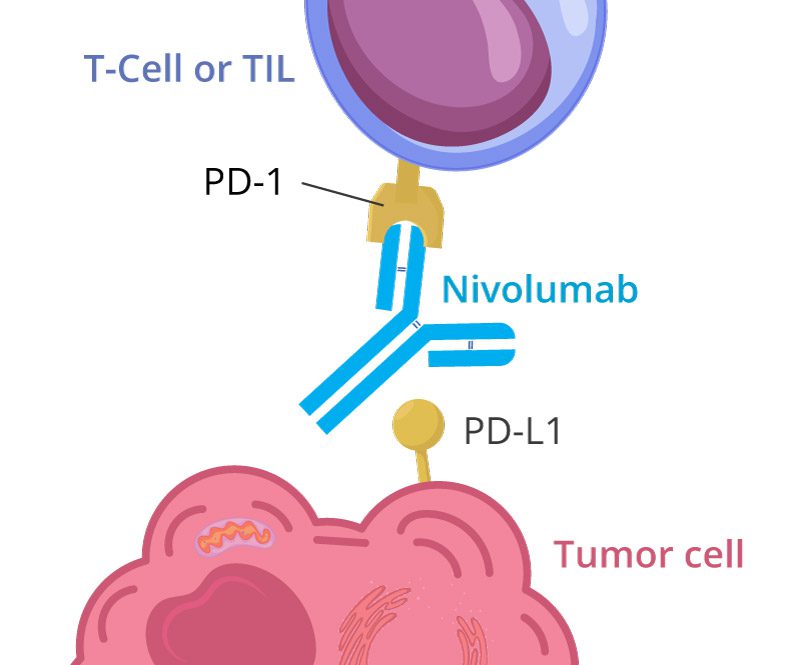
The main target of Nivolumab (brand name is Opdivo) is the Program Death protein (PD-1). Many immune cells have this receptor, the active form of which works as a brake for an immune response.
Negative Checkpoint Proteins
Imagine a cancer cell is put on trial. There is positive evidence that screams “guilty,” helping prosecutors cell to lay down a compelling case:
- Genetic mutations,
- Hijacked signaling pathways,
- Angiogenesis
At the same time, there is always confusing evidence, perhaps even some that whispers “not guilty”—at least, not entirely.
Negative checkpoint proteins comprised a latter group, and for tumor cells, they can play the role of “Devil’s advocate“, helping them to evade prosecution.
There are several types of negative checkpoint proteins, with PD-1 and CTLA-4 primary targets of novel anti-cancer drugs.
Program Death Protein 1 (PD-1)
The PD-1 receptor is a transmembrane protein comprising 288 amino acids. It is normally present on various immune cells, playing a huge role in the upregulation of an immune response:
- B cells – the main type of antibody-producing cells;
- T cells – part of the adaptive immune response, “elite forces” of your immune system, which receive training to recognise and eliminate bugs;
- Natural killer (NK) cells usually represent the first line of defence.
One particular subtype of T-cells, called Tumor-Infiltrating Lymphocytes (TIL), expresses abundant quantities of PD-1 receptors on their surface. TILs are responsible for finding and killing suspicious cancer-like cells in your body. This natural cancer monitoring tool is highly effective, cleaning around 20 cancer cells each day.
How Does Cancer Immunity Work
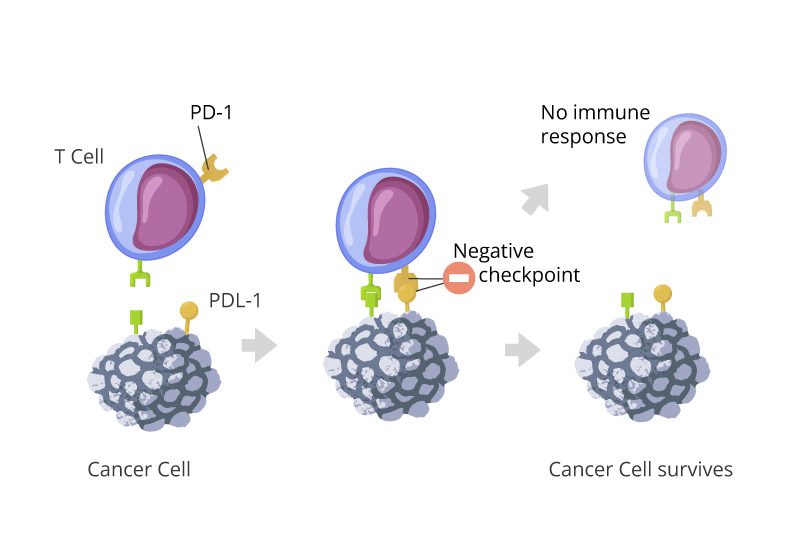
The immune system works around the clock to find abnormal cells. TILs monitor billions of cells to check if they have any suspicious features – special proteins that might suggest these cells harbor some cancer traits and can potentially be a threat to the host.
Imagine every second, TILs conduct a risk survey, analyzing both positive and negative evidence, before making a decision.
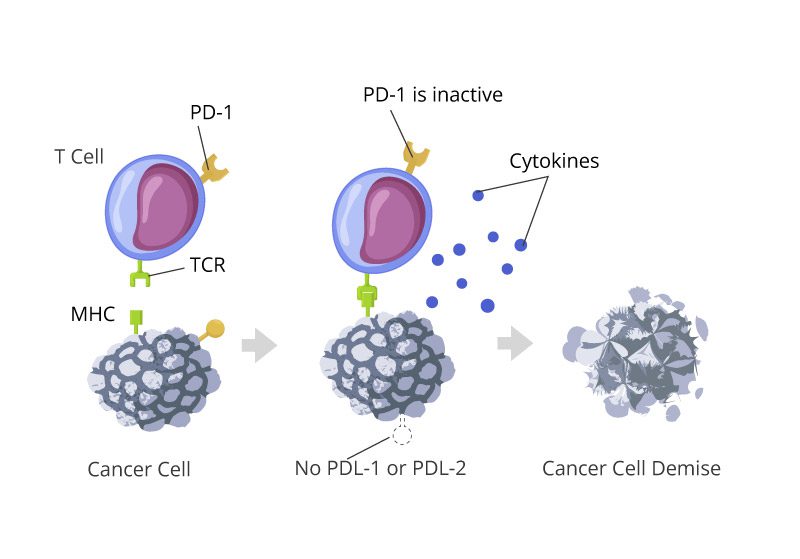
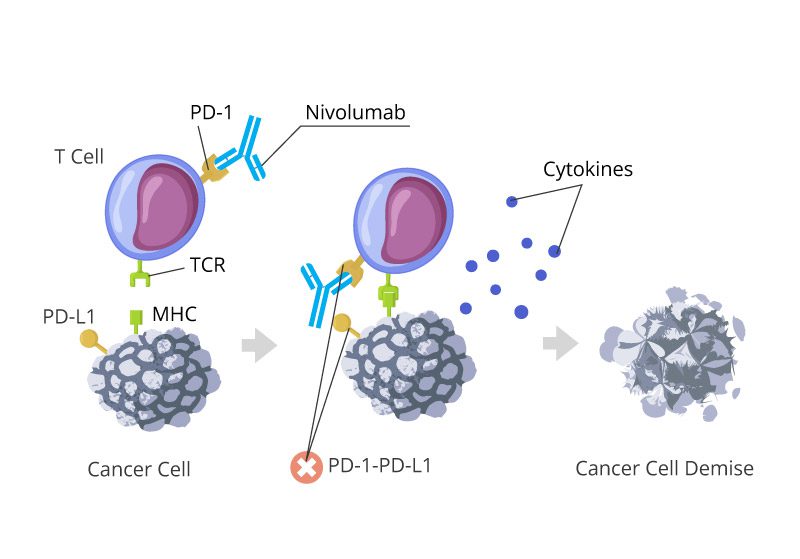
If the evidence is overwhelmingly positive, the cells would be destroyed. One of those whistle-blowers is TCR (T-cell receptor), alerting the immune system of potential abnormalities such as cancerous major histocompatibility complex (MHC).
On the other side of the scale is a PD-1, which works as a cell’s best advocate. In the case of melanoma, it is an advocate of the devil.
By binding to the PD-1 receptor of cancer-killing cells, Nivolumab blocks one of the most important ways for tumor cells to escape the immune radar and evade the prosecution.
Nivolumab, in nutshell is cancer anti-sparing medicine, helps immune system to be a tune for any suspects.
Another prominent PD-1 inhibitor is Pembrolizumab, better known under the brand name Keytruda.
PD-1 and cancer cells
Cancers have a few tricks to slip from the radar of the immune system.
Activating PD-1 is crucial for the survival of many cancers, like melanoma, renal cell carcinoma, astrocytoma, or colorectal cancer.
To activate a “negative checkpoint,” they all express two types of Program Death Ligands – PD-L1 and PD-L2.
Once the immune cell comes closer to inspect a the cancer one, the ligand PD-L1 would activate a PD-1, keeping tumor cells out of suspicion.
PD-L1 in tumors
According to the research, only one in three cancers express PD-L1. Particularly, some solid tumors are pretty good at producing the ligands on the surfaces of their cells:
- an ovarian cancer;
- a melanoma;
- a lung cancer.
PD-L2 in tumors
PD-L2, having a similar structure to PD-L1, creates a better and stronger bond with PD-1. Studies estimate the binding affinity of PD-L2 is two to sixfold higher.
PD-L2 is found in many epithelial cancers and B-cell lymphomas.
How does Nivolumab bind the PD-1?
Paul Gauguin, a famous painter, once told his friend Bernard: “Do not copy nature. Art is an abstraction”. Although much of the art history of the 20th century proved it was worthy of advice, modern scientists still consider imitation to be one of the greatest tools in their arsenal.

Nivolumab is a mere antibody. Our immune system produces billions of them each day to eliminate unwanted and harmful agents. A few things make Nivolumab special:
- It is monoclonal (mAb) – all copies of it have the same structure and represent the same class and a serotype of IgG.
- It is fully human – the structure is identical to a normal human antibody, which helps to stay longer in our bodies without eliciting our immune reaction.
- It belongs to the family of immune checkpoint inhibitors.
- It binds to a Program Death protein 1 with affinity and specificity. A single dose of nivolumab can link up to around 85% of all PD-1 receptors, and after 24 hours, around 70%.
When Nivolumab connects to the PD-1 receptor on a T-cell or NK-cell it blocks PD-1’s ability to couple with PD-L1 or PD-L2, preventing a cancer cell from abusing this evasion route and getting off the immune radar.
What Cancers Can Nivolumab Treat?
Nivolumab was developed by Bristol-Myers Squibb and received FDA approval in 2014, initially for treating metastatic melanoma.
Over time, its applications expanded to cover multiple cancers:
1. Melanoma
Nivolumab was first approved for unresectable or metastatic melanoma. It demonstrated high efficacy, particularly in cases where other treatments failed.
2. Non-Small Cell Lung Cancer (NSCLC)
A significant milestone in the treatment of NSCLC, Nivolumab has shown effectiveness in patients with advanced or metastatic disease, especially after the failure of chemotherapy.
3. Renal Cell Carcinoma (RCC)
For advanced kidney cancers, Nivolumab improved overall survival rates compared to previously established treatments like everolimus.
4. Head and Neck Squamous Cell Carcinoma (HNSCC)
Nivolumab is particularly beneficial for recurrent or metastatic HNSCC with progression on or after platinum-based therapy.
5. Classical Hodgkin Lymphoma (cHL)
The ability of Nivolumab to respond to immune-evasive hematological cancers, such as cHL, has expanded its utility in hematological oncology.
6. Colorectal Cancer (CRC)
Certain CRC cases with mismatched repair deficiency (dMMR) respond well to Nivolumab due to high mutational burden, making the tumors more “visible” to the immune system.
What Are the Side Effects of Nivolumab?
Like all therapies, Nivolumab carries potential risks. Its immune system activation can lead to immune-related adverse events (irAEs), affecting both efficacy and tolerability. Below are some common and rare side effects:
Common Side Effects:
- Fatigue
- Rash and skin reactions such as pruritus
- Diarrhea or colitis
- Musculoskeletal pain
- General fever or flu-like symptoms
Immune-Related Adverse Events (irAEs):
These occur due to heightened immune activity and may involve any organ system. Examples include:
- Lungs (Pneumonitis). If you are short on breath or have a persistent cough, please let your doctor know, as Nivolumab might increase the risks of your lung tissues being damaged.
- Liver (Hepatitis): your doctor will check your liver function tests to ensure the enzymes are not elevated
- Endocrine Disorders: Some normal endocrine cells express small quantities of PDL-1 and can be targeted by the immune system. Although recent studies haven’t found a link between PDL-1 expression and endocrine complications of nivolumab treatment, the doctor might check the levels of thyroid or pituitary hormones and request an ultrasound or MRI to check up on your glands.
- Gut (Colitis): in rare cases, severe inflammation of the digestive tract may develop, prompting your doctor to check your stool for potential inflammatory signs or request a colonoscopy.
While these side effects are typically manageable, it’s essential to let your doctor ASAP if you experience any problems and do your prescribed routine tests on time.

Leave a Reply